Introduction
Physical therapy in Frankfort, New Lenox for Hand Conditions
Welcome to JointPro Physical Therapy's guide to Finger Fusion.
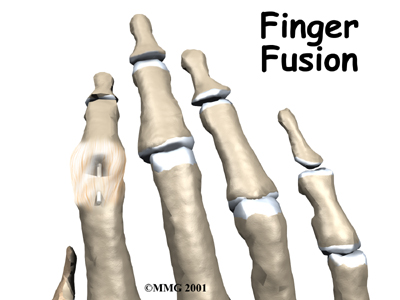
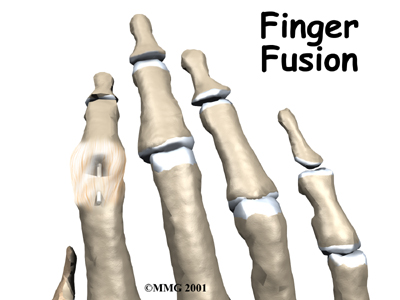
Arthritis of the finger joints may be surgically treated with a fusion procedure. A fusion keeps the problem joints from moving so that pain is eliminated.
This guide will help you understand:
- what parts make up the finger joint
- why this type of surgery is used
- how the operation is performed
- what to expect before and after surgery
- JointPro Physical Therapy’s guide to rehabilitation after surgery
Anatomy
 What parts of the finger are involved?
What parts of the finger are involved?
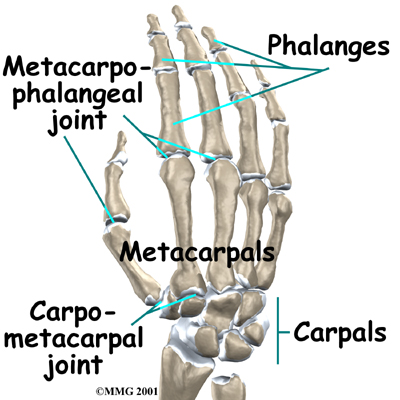
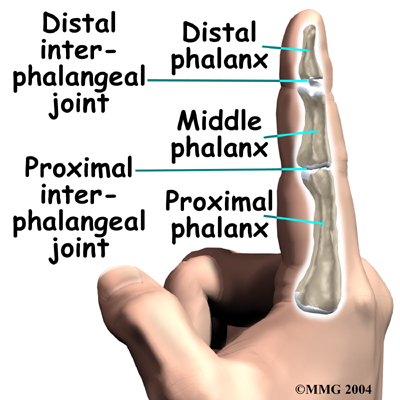
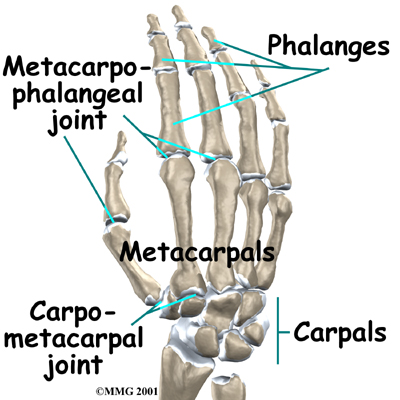
The finger joints work like hinges when the fingers bend and straighten. The main knuckle joint is the metacarpophalangeal joint (MCP joint). It is formed by the connection of the metacarpal bone in the palm of the hand with the finger bone, or phalange. Each finger (the thumb is not termed a finger) has three phalanges, separated by two interphalangeal joints (IP joints. The closest phalange to the MCP joint (knuckle) is called the proximal IP joint (PIP joint). The joint near the end of the finger is called the distal IP joint (DIP joint).
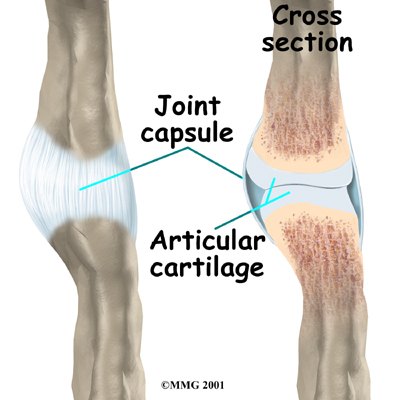
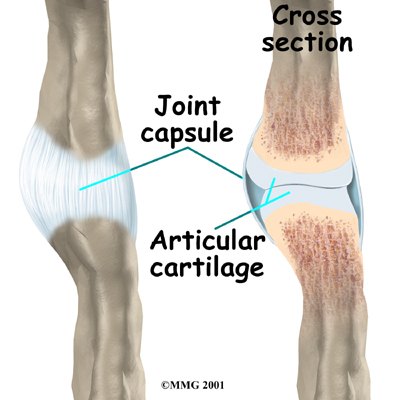
Ligaments are tough bands of tissue that connect bones together. Several ligaments hold the joints together in the finger. These ligaments join to form the joint capsule of the finger joint, a watertight sac around the joint. The joint surfaces are covered with a material called articular cartilage. This material is the slick, spongy covering that allows one side of a joint to slide against the other joint surface easily. When this material wears out, the joint develops a type of arthritis called osteoarthritis and becomes painful. Rheumatic arthritis is a different form of arthritis (which is more widespread in the body and develops due to an autoimmune disorder) but can also cause wearing out of the joint surfaces and deformity of the joints.
Related Document: JointPro Physical Therapy's Guide to Hand Anatomy
Hand Anatomy Introduction
Rationale
Why is a finger joint fused?
Arthritic finger joints cause pain and make it difficult to perform normal movements, such as grasping and pinching. Advanced arthritis can also loosen the joint and may begin to cause finger joint deformity. Joint fusion is a procedure that binds the two joint surfaces of the finger together, keeping them from rubbing on one another. Fusing the two joint surfaces together relieves pain, makes the joint stable, and prevents additional joint deformity. It is used when all other potential forms of treatment, including finger joint replacement, have been exhausted.
Preparation
What should I do to prepare for surgery?
The decision to proceed with surgery must be made together by you and your surgeon. Your physical therapist may also liaise with your surgeon to confirm the types of therapy techniques trialed and confirm the ineffectiveness of conservative therapy. You need to understand as much about the procedure as possible. Any concerns or questions you have should be brought up to your surgeon.
Once you decide to go ahead with the surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn't eat or drink anything after midnight the night before. The length of time you spend in the hospital depends on a variety of factors including the ease of the surgery, your body’s reaction to the surgery, as well as any complications that can, but rarely occur.
Surgical Procedure
What happens during the operation?
 Surgery can last up to 90 minutes. Surgery may be done using a general anesthetic, which puts you completely to sleep, or a local anesthetic, which numbs only the hand. With a local anesthetic you may be awake during the surgery, but you won't be able to see the surgery.
Surgery can last up to 90 minutes. Surgery may be done using a general anesthetic, which puts you completely to sleep, or a local anesthetic, which numbs only the hand. With a local anesthetic you may be awake during the surgery, but you won't be able to see the surgery.
Once you have had the anesthesia, your surgeon will make sure the skin of your hand is free of infection by cleaning the skin with a germ-killing solution.
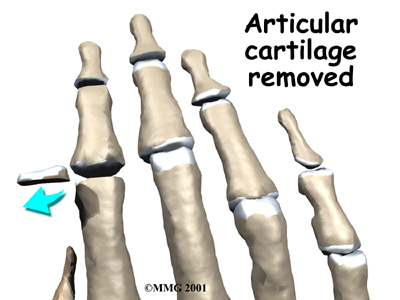
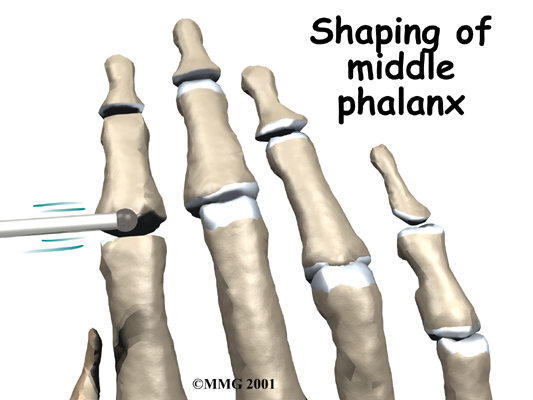
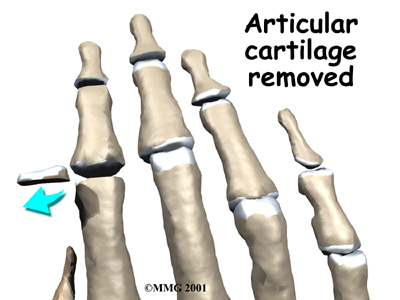
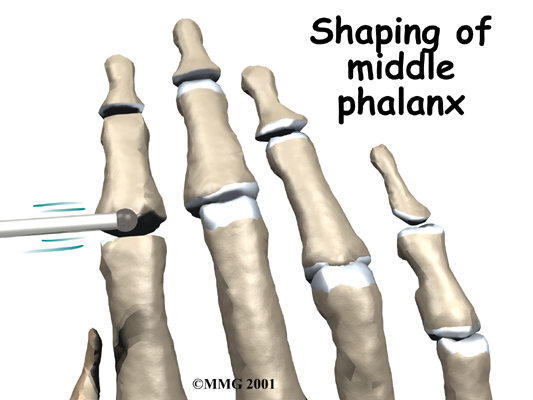
An incision is made on the back part of the finger over the surface of the joint that is to be fused. Special care is taken not to damage the nearby nerves going to the finger. The joint capsule surrounding the finger joint is then opened so that the surgeon can see the joint surfaces. The articular cartilage is removed from both joint surfaces to leave two surfaces of raw bone. The bottom of the phalange is hollowed with a special tool to form a socket. The other surface is shaped into a rounded cone that fits inside the socket.
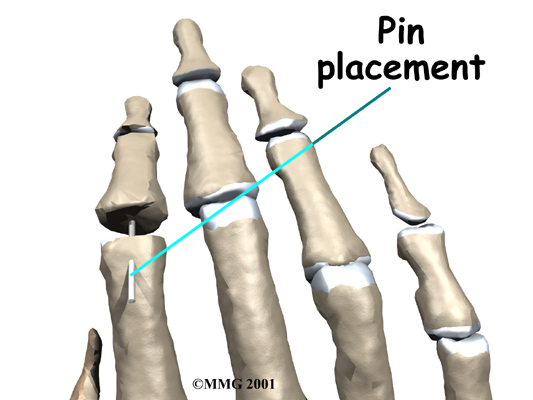
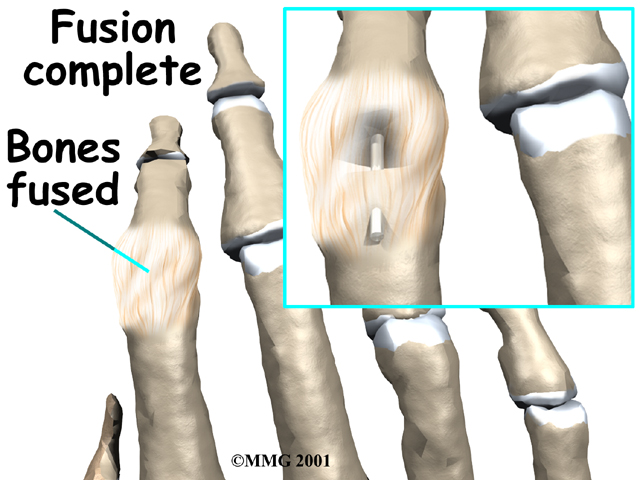
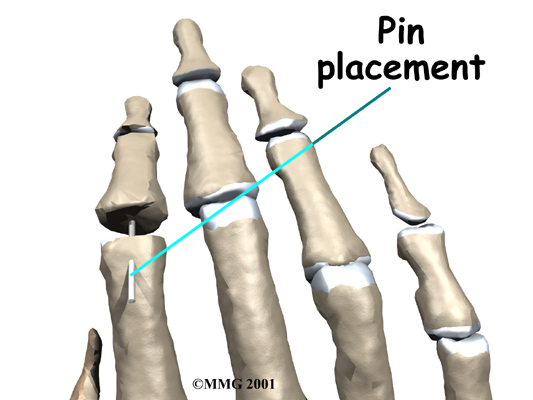
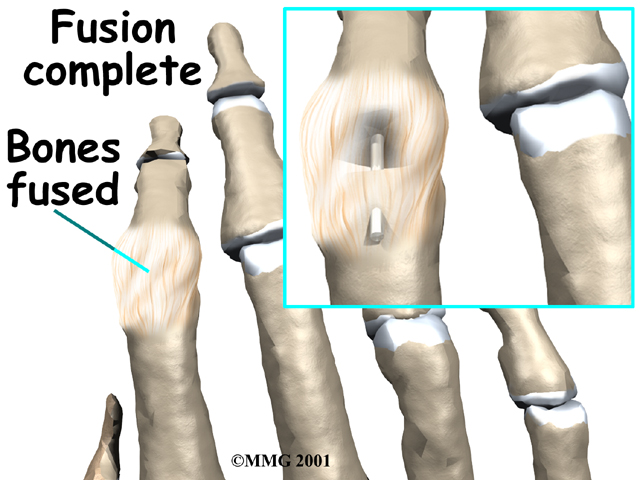
The surgeon places a metal pin through the center of both bones and then connects the cone and socket snugly together. The metal pin allows the surgeon to hold the two bones in the correct alignment and prevents the bones from moving too much as they grow together, or fuse.
The soft tissues over the joint are sewn back together. The forearm and hand are then placed in a cast until the bones completely fuse together. This takes about six weeks.
After Surgery
What happens immediately after surgery?
After surgery, you will wear an elbow-length cast for about six weeks. This gives the ends of the bones time to fuse together. Your surgeon will want to check your hand in five to seven days. Stitches may need to be removed after 10 to 14 days, though most of your stitches will be absorbed into your body. You may have some discomfort after surgery. You will be given pain medication by your doctor to control the discomfort.
You should keep your hand elevated above the level of your heart for several days to avoid swelling and throbbing. Keep it propped up on a stack of pillows when sleeping or sitting up. Ice may also be used at this stage for pain relief.
Rehabilitation
What should I expect during my rehabilitation period?
As mentioned above, you will wear a cast on your arm and hand for about six weeks to give the fusion time to heal. When the cast is removed, you may have stiffness or pain in the joints closest to the fused joint or pain around the surgical incision. physical therapy at JointPro Physical Therapy will help relieve your pain and decrease the stiffness in the surrounding joints.
In order to decrease pain we may use modalities such as heat, ice, or electrical current.
These will assist with managing pain and any ongoing swelling you have around the surgical site, anywhere along the arm, or into the hand. Massage to these areas may also be done in order to improve circulation and assist with easing any discomfort. Some of the muscles of the neck may also be painful from having the arm in a cast for an extended period. These muscles may also benefit from massage treatment, which will make movement of your entire surgical side easier.
The next part of our treatment will focus on regaining the range of motion, strength, and dexterity in the joints on either side of your fused finger as well as your other fingers, wrist, hand, elbow, and even shoulder. As the motion of your fused joint will be permanently lost, it is of paramount importance to maintain the range of motion, strength, and dexterity in the joints surrounding the fusion in order to be able to continue to use your hand functionally. Your physical therapist at JointPro Physical Therapy will prescribe a series of range of motion and strengthening exercises that you will practice in the clinic and also learn to do as part of your home exercise program. These exercises may include the use of rehabilitation equipment such as mini pulleys, putty, elastics or balls for strengthening and gripping resistance. In addition to strengthening your grip we will educate you on ways to grip and support items in order to do your daily tasks by compensating for your surgical finger but without putting too much stress on your healing fusion or the other joints.
If necessary, your physical therapist will mobilize the joints above and below your fused joint or any other joint in the area that is stiff and impeding movement of your hand and limb. This hands-on technique encourages the stiff joints to move gradually into their normal range of motion.
Being able to move your hand and finger so that you can complete your work tasks and daily activities is the goal for our therapy at JointPro Physical Therapy. Maximizing dexterity can greatly improve the functional use of your hand. For this reason, we will also incorporate functional activities like picking up items from a table or twisting items into place using your surgical hand. These functional activities encourage the joints and the muscles of the hand and arm to work in unison, which is critical to maximizing the use of your overall upper limb. Exercises where weight is put through your fused joint, such as pressing the pad of your finger into something, will also be added when appropriate to encourage the fusion to tolerate weight in a controlled fashion.
When you are well underway, regular visits to JointPro Physical Therapy will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program. Generally, the majority of your gains from physical therapy will occur within the first 1-2 months after the joint is fused. Since the fused joint does not move and therefore does not need any therapy to gain range of motion itself, improvements with therapy at JointPro Physical Therapyafter a finger joint fusion are noticed very quickly.
Generally the physical therapy we provide at JointPro Physical Therapy after finger joint fusion occurs without any complications. If, however, during rehabilitation your pain continues longer than it should or therapy is not progressing as your physical therapist would expect, we will ask you to follow-up with your surgeon to confirm that the joint fusion is tolerating the rehabilitation well and to ensure that there are no hardware issues that may be impeding your recovery.
JointPro Physical Therapy provides services for physical therapy in Frankfort, New Lenox.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications with a fusion of the finger are highlighted below:
- reaction to the anesthesia
- infection
- nerve damage
- nonunion
Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs that the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss these risks and your concerns with your anesthesiologist.
Infection
Any operation carries a small risk of infection. Fusing the finger joint is no different. You will probably be given antibiotics before the operation to reduce the risk of infection. If an infection occurs you will most likely need antibiotics to cure it. You may need additional operations to drain the infection if it involves the area around the hardware. In these cases, the hardware may need to be removed.
Nerve Damage
All of the nerves and blood vessels that go to the finger travel across, or near, the finger joint. Since the operation is performed so close to these important structures, it is possible to injure either the nerves or the blood vessels during surgery. The result may be temporary if the nerve injury has come from the nerve being stretched by retractors during the surgery holding them out of the way. It is uncommon to have permanent injury to either the nerves or the blood vessels during this surgery, but it is possible.
Nonunion
Sometimes the finger bones do not fuse as planned. This is called a nonunion, or pseudarthrosis. (Pseud means false, and arthro means joint; a pseudarthrosis refers to the motion at a false joint.) If the motion from a nonunion continues to cause pain, you may need a second operation to try to get the bones to completely fuse. This may mean adding a bone graft and making sure that any metal pins that have been used are holding the bones still to allow the fusion to occur.
Portions of this document copyright MMG, LLC.








 What parts of the finger are involved?
What parts of the finger are involved?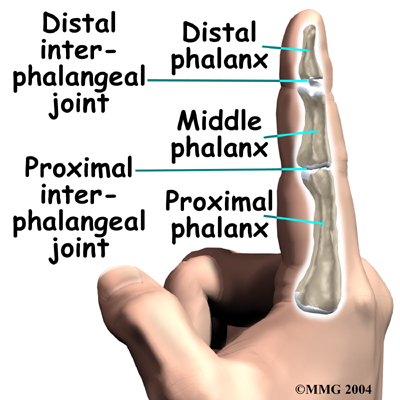
 Surgery can last up to 90 minutes. Surgery may be done using a general anesthetic, which puts you completely to sleep, or a local anesthetic, which numbs only the hand. With a local anesthetic you may be awake during the surgery, but you won't be able to see the surgery.
Surgery can last up to 90 minutes. Surgery may be done using a general anesthetic, which puts you completely to sleep, or a local anesthetic, which numbs only the hand. With a local anesthetic you may be awake during the surgery, but you won't be able to see the surgery.